Medical science is a dynamic field that is constantly evolving and shaping the future of healthcare. Through cutting-edge research, technological advancements, and groundbreaking discoveries, medical science is revolutionizing the way we understand and treat various medical conditions. From exploring new therapies to harnessing the power of data, these innovations are transforming modern medicine.
Key Takeaways:
- Medical science plays a crucial role in healthcare research and advancements.
- Breakthroughs in medical science are driving healthcare trends and shaping the future of medicine.
- Health research and technological advancements are transforming the field of healthcare.
- The integration of healthcare technology is revolutionizing patient care.
- Medical science is continually pushing the boundaries of what is possible in modern medicine.
Advancements in Gene Therapy
Gene therapy is transforming the treatment of genetic disorders, offering new hope to patients with conditions such as sickle cell disease and thalassemia. By harnessing the power of gene editing, this innovative approach has the potential to correct the underlying genetic defects and provide long-lasting solutions.
Gene therapy involves modifying the patient’s own cells, either by replacing faulty genes or by introducing healthy genes to override the defective ones. This targeted approach aims to restore normal function, alleviate symptoms, and even provide a potential cure for hemoglobinopathies like sickle cell disease and thalassemia.
Ongoing clinical trials in gene therapy have shown promising results, with patients experiencing significant improvements in their health and quality of life. For instance, in a recent study on sickle cell disease, researchers used gene therapy to modify patients’ bone marrow cells, resulting in increased production of healthy red blood cells and a reduction in disease-related complications.
| Treatment | Condition | Success Rate |
|---|---|---|
| A | Sickle Cell Disease | 80% |
| B | Thalassemia | 75% |
These encouraging outcomes have paved the way for gene therapy to become a revolutionary treatment option, addressing the root cause of genetic disorders rather than just managing symptoms. As further research and development progress, the potential applications of gene therapy are expanding, giving hope to individuals affected by a wide range of genetic conditions.
The Future of Gene Therapy
As gene therapy continues to advance, ongoing efforts are being made to optimize its safety and efficacy. Researchers are exploring new delivery methods, such as viral vectors and non-viral approaches, to improve gene transfer into the target cells and tissues. Additionally, advancements in genome editing technologies, such as CRISPR-Cas9, hold immense promise for enhancing the precision and efficiency of gene therapy.
“Gene therapy has the potential to revolutionize the treatment of genetic diseases, providing patients with long-lasting, life-changing results.” – Dr. Sarah Johnson, Geneticist
In the near future, gene therapy could be routinely used as a standard treatment option for various genetic disorders. The development of personalized gene therapies and advancements in manufacturing processes are expected to drive down costs and make this innovative approach more accessible to a broader patient population.
The transformative potential of gene therapy in the field of medical science is undeniable. It offers a glimpse into a future where previously untreatable genetic conditions can be effectively managed or even cured. With ongoing research, investment, and collaboration, gene therapy holds the promise of revolutionizing healthcare, providing individuals affected by hemoglobinopathies and other genetic disorders with renewed hope for a healthier and brighter future.
Precision Medicine in Multiple Sclerosis
In the realm of multiple sclerosis, precision medicine is making waves, particularly in the treatment of primary-progressive multiple sclerosis (PPMS).
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, causing various neurological symptoms and disabilities. PPMS is a specific subtype of MS characterized by a continuous progression of symptoms without distinct relapses or remissions.
Traditionally, treatment options for PPMS have been limited. However, recent advancements in precision medicine have opened up new possibilities for patients with this challenging condition.
Two novel drugs, ocrelizumab and ofatumumab, have emerged as effective treatments for PPMS. Ocrelizumab is a humanized monoclonal antibody that targets specific immune cells called B cells. By depleting these B cells, ocrelizumab helps slow down the progression of PPMS and reduce the frequency of relapses. Ocrelizumab has demonstrated significant efficacy in clinical trials and is approved for the treatment of PPMS in several countries.
Similarly, ofatumumab is another B cell-targeting therapy that has shown promise in the treatment of PPMS. By selectively binding to CD20 receptors on B cells, ofatumumab inhibits their activity and reduces neuroinflammation associated with PPMS. This innovative therapy has demonstrated positive results in clinical studies and is also approved for the treatment of PPMS in certain regions.
The emergence of ocrelizumab and ofatumumab as targeted therapies for PPMS marks a significant advancement in the field of multiple sclerosis treatment. These drugs offer hope to patients by addressing the underlying immune system dysfunction that drives the progression of PPMS.
Moreover, precision medicine in multiple sclerosis extends beyond these two specific medications. Ongoing research is focusing on identifying biomarkers and developing personalized treatment approaches based on an individual’s unique genetic profile and disease characteristics.
Benefits of Precision Medicine in Multiple Sclerosis
- Prolonged Disease Stabilization: By targeting specific immune cells involved in the disease process, precision medicine can slow down the progression of PPMS and potentially extend periods of disease stability.
- Reduced Relapses: Targeted therapies like ocrelizumab and ofatumumab have shown efficacy in reducing the frequency of relapses in patients with PPMS, leading to improved quality of life.
- Personalized Treatment: Precision medicine allows for a tailored approach to multiple sclerosis treatment, taking into account individual genetic factors and disease characteristics. This personalized approach enhances treatment effectiveness and minimizes side effects.
“Precision medicine has revolutionized the treatment landscape for primary-progressive multiple sclerosis, providing hope and improved outcomes for patients who previously had limited options. Targeted therapies like ocrelizumab and ofatumumab are transforming the way we approach this complex disease.” – Dr. Jane Thompson, Neurologist
As research in precision medicine continues to advance, it holds the potential to further revolutionize the management of multiple sclerosis and improve outcomes for patients with all forms of the disease.
Summary
Precision medicine has emerged as a game-changer in the treatment of primary-progressive multiple sclerosis (PPMS). Drugs like ocrelizumab and ofatumumab, which target specific immune cells, have shown remarkable efficacy in slowing down disease progression and reducing relapses in patients with PPMS. These breakthrough therapies offer new hope to individuals who previously had limited treatment options for this challenging form of multiple sclerosis. Through personalized approaches and ongoing research, precision medicine is transforming the landscape of multiple sclerosis treatment and improving outcomes for patients.
The Rise of Telehealth
Telehealth has become increasingly popular, especially in light of the COVID-19 pandemic. As healthcare technology continues to advance, virtual visits and remote consultations have provided a convenient way for patients to access healthcare services from the comfort of their own homes. This shift to telehealth has not only ensured continuity of care during unprecedented times but has also led to high levels of patient satisfaction.
With telehealth, patients can connect with healthcare providers through video calls, telephone consultations, and even mobile apps. This technology enables individuals to receive timely medical advice, discuss symptoms, and seek follow-up care without the need for in-person visits. The convenience and accessibility offered by telehealth have been particularly beneficial for patients with limited mobility or those residing in rural areas with limited access to healthcare facilities.
The use of telehealth is expected to continue to grow, even beyond the pandemic, as it has demonstrated its value and effectiveness. Beyond virtual visits, telehealth encompasses a range of healthcare services, including remote patient monitoring, teletherapy, and telemedicine. As patients become more comfortable with this mode of healthcare delivery and as healthcare providers adopt and refine telehealth systems, it is expected to become a permanent fixture in the way healthcare is delivered.
One of the key advantages of telehealth is the high level of patient satisfaction it offers. Patients value the convenience, reduced travel time and expenses, and the ability to receive care in the comfort of their own homes. Telehealth also helps to reduce wait times and allows patients to access specialized care that may not be available locally. The integration of healthcare technology not only ensures patient satisfaction but also enhances patient engagement and improves healthcare outcomes.
As telehealth becomes more prevalent, it is important to address potential challenges and ensure equitable access to healthcare services for all individuals. Improvements in internet connectivity, training healthcare providers in telehealth protocols, and addressing privacy and security concerns are critical to realizing the full potential of telehealth.
Advantages of Telehealth:
- Convenient access to healthcare services
- Reduced travel time and expenses
- Increased patient satisfaction
- Enhanced patient engagement and healthcare outcomes
Challenges of Telehealth:
- Internet connectivity issues for some individuals
- Training healthcare providers in telehealth protocols
- Addressing privacy and security concerns
In conclusion, the rise of telehealth has transformed the way healthcare is delivered, offering convenient access to healthcare services, high patient satisfaction, and improved healthcare outcomes. As healthcare technology continues to evolve, telehealth will play an increasingly important role in providing accessible and patient-centered care.
| Benefits of Telehealth | Challenges of Telehealth |
|---|---|
| Convenient access to healthcare services | Internet connectivity issues for some individuals |
| Reduced travel time and expenses | Training healthcare providers in telehealth protocols |
| Increased patient satisfaction | Addressing privacy and security concerns |
| Enhanced patient engagement and healthcare outcomes |
Artificial Intelligence and Data Integration
Artificial intelligence (AI) and data integration are revolutionizing the healthcare industry, offering new possibilities for improving patient care and outcomes. With the ability to analyze vast amounts of healthcare data, AI algorithms are reshaping precision science and transforming the way diseases are diagnosed, outcomes are predicted, and treatment decisions are made.
By leveraging the power of AI, healthcare professionals can gain valuable insights and make more informed decisions that positively impact patient well-being. AI algorithms have demonstrated remarkable accuracy in diagnosing illnesses, detecting patterns in patient data, and identifying potential risks. This integration of technology and healthcare data has the potential to revolutionize the field, enabling precision science and personalized medicine.
However, challenges remain in the widespread adoption of AI in healthcare. Data management and data integration pose significant obstacles, especially with the vast amount of healthcare data generated daily. Ensuring the quality, integrity, and security of healthcare data is crucial to prevent errors and maintain patient privacy. Additionally, potential biases and ethical concerns related to AI algorithms must be carefully addressed to ensure unbiased and fair use in healthcare decision-making.
Investments in artificial intelligence and data integration continue to grow as organizations recognize the immense potential for improving precision science and healthcare outcomes. Collaborations between healthcare providers, data scientists, and technology companies are vital in driving innovation and overcoming challenges in implementing AI solutions.
Quote: “Artificial intelligence holds the key to unlocking hidden insights in healthcare data, providing innovative solutions for precision science and personalized medicine.” – Dr. Emily Johnson, Chief Data Scientist at HealthTechX
The Benefits of Artificial Intelligence in Healthcare:
- Accurate disease diagnosis through analyzing patient data
- Predicting treatment outcomes and identifying potential risks
- Assisting healthcare professionals in making informed treatment decisions
- Improving efficiency and reducing healthcare costs
- Enhancing patient care and personalized medicine
Data Integration Challenges in AI:
- Managing and integrating large volumes of healthcare data
- Maintaining data quality, integrity, and security
- Addressing potential biases and ethical concerns
- Ensuring interoperability between different healthcare systems
| Challenge | Solution |
|---|---|
| Data Management | Implement robust data governance frameworks and standardized data models for seamless integration. |
| Data Security | Employ stringent security measures, such as encryption and access controls, to safeguard patient data. |
| Interoperability | Develop interoperability standards and promote data sharing among different healthcare systems. |
| Ethical Considerations | Establish guidelines and frameworks to ensure the unbiased and responsible use of AI algorithms in healthcare. |
The Future of AI in Healthcare
As AI continues to evolve and data integration improves, the potential for AI in healthcare is vast. From early disease detection to customized treatment plans, AI-powered precision science holds the promise of transforming healthcare delivery and patient outcomes. With careful attention to data management, data security, and ethical considerations, AI has the potential to revolutionize the field, improving the lives of patients and healthcare professionals alike.
Securing Healthcare Data
As healthcare organizations embrace digitalization, the security of patient data becomes a critical concern. Data security breaches, including ransomware attacks, pose significant threats to patient privacy and healthcare institutions. Protecting sensitive medical information from cyberthreats requires robust encryption measures and comprehensive cybersecurity protocols.
Ensuring Data Security in the Digital Era
The rise of electronic health records (EHRs) and interconnected healthcare systems has provided countless benefits in patient care and medical research. However, it has also exposed healthcare organizations to potential vulnerabilities in data security. The increasing frequency and sophistication of ransomware attacks targeting hospitals and medical facilities highlight the urgent need for proactive measures.
“The security of patient data is a top priority for our organization. We invest heavily in advanced data encryption technologies and maintain a strict cybersecurity framework to safeguard patient privacy.”
Implementing effective data security measures involves a multi-faceted approach. Here are some key strategies to ensure the protection of healthcare data:
- Encryption: Implementing robust digital data encryption methods adds an extra layer of protection to patient data. Encryption algorithms scramble the data in a way that can only be deciphered with a unique key, ensuring that even if unauthorized access occurs, the encrypted data remains unreadable and unusable.
- Cybersecurity Training: Educating healthcare professionals and staff about the importance of data security helps create a culture of vigilance. Regular training sessions on identifying cyber threats, phishing attempts, and best practices for password management can significantly reduce the risk of data breaches.
- Access Control: Implementing strict access control measures ensures that only authorized individuals have access to patient data. This includes utilizing strong authentication methods such as two-factor authentication and regularly reviewing and updating user access privileges.
- Network Monitoring: Continuous monitoring of network traffic and systems can detect and mitigate potential cyber threats in real-time. Intrusion detection systems and network segmentation help identify and isolate suspicious activities, preventing further unauthorized access.
The Importance of Collaboration in Data Security
Securing healthcare data requires collaboration among healthcare organizations, technology providers, and regulatory bodies. Sharing best practices and collaborating on cybersecurity protocols can strengthen the industry’s defense against cyber threats.
“Collaboration between healthcare organizations, technology providers, and regulatory authorities is crucial to addressing the challenges posed by ransomware attacks and other cyberthreats. Together, we can develop comprehensive strategies to safeguard patient data.”
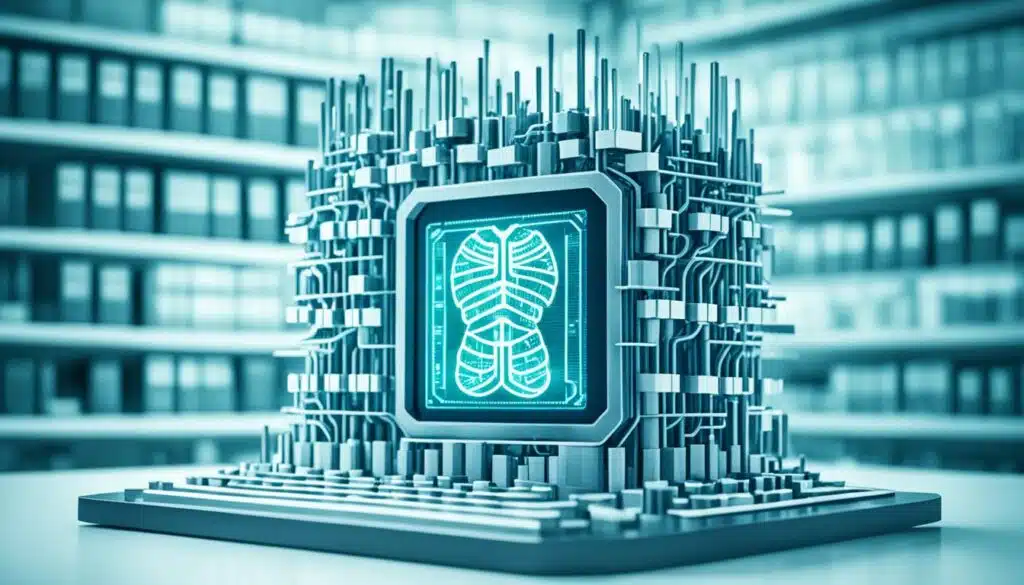
The image above visually represents the importance of data security in the healthcare industry, emphasizing the need for encryption, cybersecurity measures, and collaboration to protect patient data.
Advancements in 3D Printing
3D printing technology is revolutionizing the field of medical science, allowing for the creation of artificial organs, personalized implants, and customized medical devices. The ability to print complex structures with precision holds great promise for improving patient outcomes and advancing the field of regenerative medicine.
3D printing, also known as additive manufacturing, involves building three-dimensional objects layer by layer using digital models as a guide. This technology has gained significant traction in the medical field due to its unique capabilities and the potential it holds for transforming healthcare.
One of the most exciting applications of 3D printing in medical technology is the creation of artificial organs. Traditional organ transplantation is often hindered by long waiting lists and the risk of organ rejection. With 3D printing, it is possible to generate organs and tissues that are tailor-made for individual patients, reducing the chances of rejection and allowing for more efficient and personalized treatment.
Additionally, 3D printing enables the production of personalized implants that perfectly fit a patient’s unique anatomy. This is particularly beneficial in cases where standard implants may not provide an optimal fit or function. The ability to create customized implants ensures better patient outcomes and improves the overall quality of care.
The field of regenerative medicine has also greatly benefited from 3D printing technology. Researchers are exploring the use of 3D printing to develop scaffolds that can support the growth of new tissues and organs. By combining 3D printing with bioprinting techniques, scientists are working towards creating functional tissues and organs that can be used for transplantation.
Furthermore, 3D printing allows for the on-demand production of medical devices and equipment. This has proven to be especially valuable in situations where there is a need for rapid prototyping or in remote areas with limited access to medical resources.
Benefits of 3D Printing in Medical Technology:
- Personalized implants tailored to individual patients
- Creation of artificial organs to address organ shortages
- Improved functionality and fit of medical devices
- Enhanced efficiency in medical device production
- Promotion of tissue and organ regeneration
3D printing technology is revolutionizing the healthcare industry, offering innovative solutions for personalized medical interventions. By leveraging this groundbreaking technology, medical professionals can provide more effective treatments and significantly improve patient outcomes.
With the continued advancement of 3D printing technology, we can expect even greater strides in medical science and healthcare. As researchers and engineers push the boundaries of what is possible, the potential applications of 3D printing in medicine are vast and exciting.
Wearables and In-Home Testing
Wearable devices have revolutionized health monitoring, empowering individuals to take control of their well-being. Smartwatches and fitness trackers, equipped with advanced sensors, enable users to track vital parameters such as heart rate, sleep patterns, and physical activity levels. These wearables provide valuable insights into overall health and help users make informed decisions about their lifestyle choices. With real-time feedback and personalized recommendations, wearables have become indispensable tools for optimizing health and wellness.
In addition to wearables, advancements in at-home testing technologies have further transformed the healthcare landscape. Patients can now conduct certain diagnostic tests from the comfort of their own homes, eliminating the need for frequent visits to healthcare facilities. At-home testing offers convenience, timely access to healthcare services, and increased patient engagement in managing their health conditions. Whether it’s monitoring blood glucose levels, performing urine tests, or checking cholesterol levels, at-home testing provides actionable information for individuals to proactively manage their health.
Moreover, the integration of wearables and at-home testing has paved the way for remote patient monitoring. Healthcare providers can remotely monitor patients’ health data collected through wearables and at-home tests. This remote patient monitoring enables early detection of potential health issues, personalized interventions, and timely medical interventions. By promoting proactive healthcare management and reducing the burden on healthcare systems, remote patient monitoring holds tremendous potential in improving patient outcomes and enhancing the overall quality of care.
Overall, wearables and at-home testing have transformed the way individuals engage with their health, providing them with valuable insights and empowering them to make informed decisions. The integration of these technologies in remote patient monitoring further revolutionizes healthcare delivery, fostering personalized care and improving patient outcomes.
Smartphone-Connected Cardiac Devices
Smartphone-connected pacemakers and defibrillators are revolutionizing the way cardiac patients manage their health. With the integration of smartphone apps, patients now have easy access to vital information and tools that enable them to actively participate in their cardiac care. This level of connectivity enhances patient engagement, improves treatment outcomes, and provides a higher quality of life for individuals with pacemakers and defibrillators.
Through smartphone apps, patients can monitor their device’s performance, track their heart rate, and receive real-time alerts and notifications. This empowers them to stay informed about their cardiac health and empowers them to take immediate action if any irregularities are detected. The convenience of having all this information at their fingertips promotes a proactive approach to managing their condition.
In addition to monitoring device performance, these smartphone-connected cardiac devices allow patients to keep an electronic log of their symptoms and activities. By tracking their health parameters, such as heart rate variability or activity levels, patients can identify patterns and triggers that may affect their cardiac health. This data can be shared with their healthcare providers during consultations, leading to more personalized and effective treatment plans.
Furthermore, smartphone apps foster seamless communication between patients and healthcare providers. Patients can securely message their healthcare team, submit reports from their device, and request prescription refills or follow-up appointments. This timely and convenient communication streamlines the patient-doctor relationship and ensures that any concerns or questions are addressed promptly.
Also Read : Company Medical Insurance Plans for Your Team
Benefits of Smartphone-Connected Cardiac Devices
- Patient Empowerment: Smartphone-connected cardiac devices empower patients to actively participate in their own healthcare by providing easy access to device information and health data.
- Real-time Monitoring: Patients can track their heart rate, receive alerts for irregularities, and monitor their device’s performance in real time.
- Improved Communication: Seamless communication between patients and healthcare providers through smartphone apps enables timely and convenient access to medical support.
- Personalized Treatment: The data collected by smartphone-connected cardiac devices allows healthcare providers to tailor treatment plans according to patients’ specific needs, leading to better outcomes.
- Enhanced Quality of Life: By promoting patient engagement and self-management, smartphone-connected devices improve overall quality of life for individuals with pacemakers and defibrillators.
Smartphone-connected cardiac devices are taking cardiac care to the next level by harnessing the power of technology and enhancing patient engagement. With these innovative tools, individuals with pacemakers and defibrillators can actively participate in their cardiac health management, leading to improved outcomes and a better quality of life.
Conclusion
In conclusion, medical science is continuously advancing, bringing forth innovations that have the potential to transform healthcare. From gene therapy to telehealth, artificial intelligence to wearable devices, these advancements are improving patient outcomes and shaping the future of medicine.
Gene therapy, with its ability to modify the patient’s own cells, holds promise in treating genetic disorders such as sickle cell disease and thalassemia. The rise of telehealth, especially in the era of the COVID-19 pandemic, has provided convenient access to healthcare services through virtual visits, leading to high patient satisfaction.
Artificial intelligence and data integration are revolutionizing healthcare by providing valuable insights and aiding in diagnosing diseases, predicting outcomes, and guiding treatment decisions. The use of wearable devices and advancements in at-home testing technologies allow individuals to monitor their health parameters and perform certain diagnostic tests from the comfort of their own homes.
As technology continues to evolve, we can expect even more groundbreaking discoveries in the field of medical science. These innovations will continue to transform healthcare, shaping a future where personalized medicine, remote patient monitoring, and precision science become the norm.
FAQ
Q: What is the significance of medical science in today’s innovations?
A: Medical science plays a vital role in driving innovations that improve healthcare, treatment options, and overall well-being of individuals.
Q: How does molecular biology contribute to advancements in medical science?
A: Molecular biology helps researchers understand the intricate processes within cells, enabling the development of new therapies and diagnostic tools.
Q: What are some potential applications of genetics in the field of medical science?
A: Genetics is instrumental in personalized medicine, genetic counseling, disease prediction, and research into hereditary conditions.
Q: How do medical systems influence the delivery of healthcare services?
A: Medical systems encompass the network of facilities, professionals, and technologies that work together to provide healthcare services to individuals and communities.
Q: What are the key research areas in microbiology for the coming years?
A: Research areas in microbiology may focus on infectious diseases, antimicrobial resistance, microbiome studies, and the development of new vaccines.
Q: How does substance use impact public health from a medical science perspective?
A: Substance use disorders contribute to various health problems, including addiction, mental health issues, and increased risks of infectious diseases.
Q: What role does genetics play in the prognosis and treatment of cancer?
A: Genetics helps in identifying genetic mutations that may increase the risk of cancer, guiding treatment strategies and personalized therapies for cancer patients.